Microwize Medical Billing: Reduce Denials and Get Paid Faster
Running a successful healthcare practice isn’t just about delivering excellent patient care—it’s also about ensuring a steady cash flow. One of the biggest challenges for providers is dealing with claim denials and delayed reimbursements. Every rejected or delayed claim means lost revenue, wasted time, and increased administrative stress. That’s where Microwize Medical Billing comes in.
Microwize specializes in helping healthcare practices streamline their billing process, reduce denials, and get paid faster. With decades of experience and a proven track record, Microwize transforms medical billing from a headache into a seamless, revenue-boosting process.
In this article, we’ll explore how Microwize’s solutions work, why they’re trusted by thousands of providers, and how partnering with them can improve your financial performance while allowing you to focus on what matters most—your patients.
Why Medical Billing Denials Hurt Your Practice
Claim denials are more than just a nuisance. They cost your practice money, time, and resources. Industry studies show that:
- Up to 30% of claims are initially denied or rejected.
- 60% of denied claims are never resubmitted.
- The average cost of reworking a denied claim is $25 to $118 per claim.
This creates a cycle of delayed cash flow, staff burnout, and reduced efficiency. Many small and mid-sized practices simply don’t have the expertise or time to manage the ever-changing billing regulations and payer requirements.
If your billing process isn’t optimized, you’re leaving money on the table.
How Microwize Helps Reduce Denials
Microwize uses a proactive, technology-driven approach to minimize claim rejections and denials. Here’s how their process works:
1. Accurate Patient Eligibility Verification
Many claims are denied because of incorrect patient insurance details. Microwize verifies eligibility upfront to ensure claims meet payer requirements before submission.
2. Clean Claims the First Time
Their billing experts review each claim for accuracy, completeness, and compliance with payer-specific rules, reducing the chance of rejection.
3. Automated Claim Scrubbing
Using advanced billing software, claims are automatically scanned for errors before submission. This extra layer of scrutiny significantly reduces denials.
4. Expert Denial Management
If a claim is denied, Microwize’s medical billing team immediately investigates the issue, corrects errors, and resubmits the claim promptly to minimize delays.
5. Staying Updated on Regulations
Healthcare billing regulations change constantly. Microwize stays on top of payer policy updates and compliance requirements so your practice doesn’t have to.
Get Paid Faster with Streamlined Billing
Microwize doesn’t just help reduce denials—they accelerate the entire revenue cycle.
- Faster claim submissions mean quicker payments.
- Real-time tracking allows you to monitor your cash flow with transparency.
- Electronic Remittance Advice (ERA) speeds up the reconciliation process.
Their process ensures your practice gets reimbursed as quickly as possible, improving financial stability and reducing the time spent chasing payments.
Why Choose Microwize for Your Medical Billing?
Microwize has over 30 years of experience in medical billing and practice management. Here’s what sets them apart:
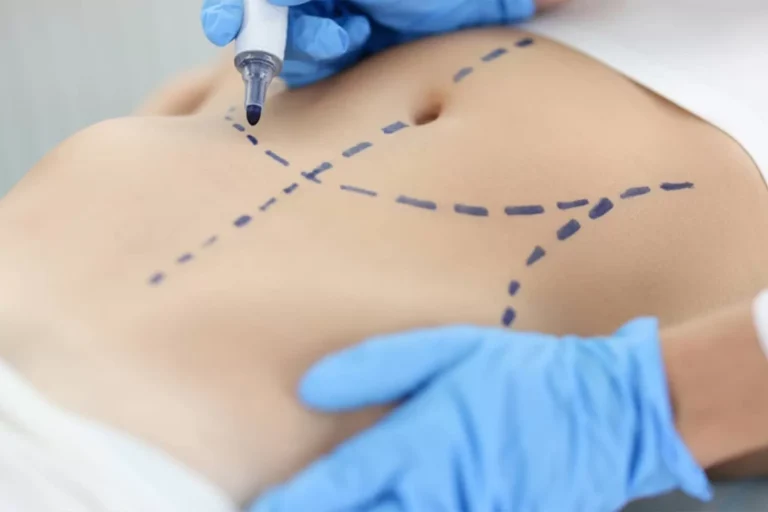
✅ Specialized Expertise – They work with all specialties, from primary care to complex surgical practices.
✅ Dedicated Support – You get a team of billing experts who understand your practice’s unique needs.
✅ Advanced Technology – Their billing software integrates with leading EHR/EMR systems for seamless workflows.
✅ Transparent Reporting – You’ll always know the status of your claims and revenue cycle performance.
✅ Affordable & Scalable – Whether you’re a solo provider or a multi-location practice, they offer flexible solutions.
By outsourcing your billing to Microwize, you free your staff from administrative burdens, reduce overhead costs, and improve profitability.
What Practices Are Saying
Healthcare providers who partner with Microwize report:
- 40% fewer claim denials
- 30% faster payment turnaround
- Significant increase in clean claim rates
- More time to focus on patient care instead of paperwork
Is Outsourcing Medical Billing Right for You?
If you’re dealing with frequent denials, delayed payments, or overwhelmed staff, outsourcing your billing might be the smartest move. Microwize allows you to:
- Focus on your patients instead of payer policies
- Gain a predictable, improved cash flow
- Ensure compliance with industry regulations
- Reduce the risk of lost revenue
Instead of hiring, training, and managing in-house billing staff, you can rely on a team of experts who specialize in maximizing reimbursements.
Take the Next Step
Claim denials don’t have to drain your practice’s revenue. By partnering with Microwize’s medical billing team, you can reduce denials, improve cash flow, and get paid faster—all while focusing on delivering quality care.
Don’t let billing challenges hold your practice back. Schedule a consultation with Microwize today and see how their proven solutions can transform your revenue cycle.
Final Thoughts
In today’s complex healthcare landscape, providers can’t afford to lose revenue due to avoidable claim denials. Microwize offers a simple, effective, and affordable way to streamline your billing process, reduce administrative headaches, and ensure your practice gets every dollar it deserves.
If you want fewer denials, faster payments, and more time for patient care, it’s time to let Microwize handle your billing with expertise you can trust.